Food Allergy Awareness Week Meets Mental Health Awareness Month
Food allergies are a physical disease with a huge impact on mental health.
May is home to Mental Health Awareness Month and Asthma & Allergy Awareness Month. These are both important issues to me, but until recently, I hadn’t spent much time thinking about their link. Sure, I know that stress can make allergies worse, as it can with most things. But I’d never considered my food allergies to be a drain on my overall mental wellbeing.
That is, until I started treatment for PTSD, due to a trauma that triggered old feelings of a friend’s suicide in college. In therapy, I began to uncover the root causes of why I had such an extreme response to trauma, and among other things, I learned my allergies were a factor.
I’d never thought about food allergies as traumatic. My first reaction was at 2.5 days old, so allergies have always been a part of my life. I wouldn’t know how to engage with the world not concerned about my diet and my potential to die from a simple ingredient mislabeling or careless restaurant chef. As it turns out, engaging in life-threatening activities on the regular (ie: eating) is not super normal and requires some processing.
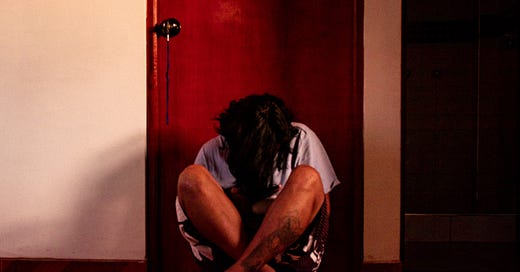
I’ve had multiple life-threatening reactions, but I’d never really taken the time to recover emotionally from them. In order to eat, I have to repress my fear of death. There are also lower-stakes situations I’ve faced that have been traumatic — bullying, going extended periods without eating, being told my allergies were an imagined experience — but that always felt like the cost of engaging socially with the world. I’d learned to accept my reality, but what I hadn’t learned to accept until recently was that it’s okay to be sad about it from time to time, and to process my experiences fully instead of bouncing right back. There’s a balance between acknowledging the trauma and mustering up the courage to eat my next meal.
I’m not alone in my experience of post-traumatic stress due to allergies. A recent study published in the March 2021 issue of Journal of Pediatric Psychology found that 81% of parents of kids with food allergies suffered from clinically significant worry and 42.3% met the clinical cut-off for PTSS — Post Traumatic Stress Syndrome. It’s important for people with food allergies, their relatives, friends, and doctors to acknowledge and understand the very real mental impact of the disease.
Everyone with food allergies should know to carry an Epi-pen at all times and have an action plan in place in case of a reaction. Similarly, access to mental health resources is critical. If you’re struggling, remember you’re not alone, and seek help, whether it’s with a therapist or through a crisis hotline; the National Suicide Prevention Lifeline is available 24/7 at 1–800–273-TALK (8255).